Module 1: Prepare for Clinical Dialogue in Primary care and In Specialty Care
Resources
Module 2: Pain Pathology and How to Apply it to One's Personal Pain Management
Resources
Module 3: The Pain Trek... What Does Progress Look Like in Pain Management?
Resources
Made possible by a grant from Collegium.
US Department of Health Pain Management Report
See Full Pain Management Report Here>>
Pain Management Fact Sheet (Patients/Families)
Pain Management Education (Veterans)
Behavioral Health & Addiction Help (Anonymous)
Pain Management Education (Veterans)
Behavioral Health & Addiction Help (Anonymous)
Patients with acute and chronic pain face a crisis because of challenges in obtaining adequate care, resulting in profound physical, emotional, and societal costs. According to the CDC, 50 million adults in the US have chronic daily pain, with 19.6 million adults experiencing high impact chronic pain that interferes with daily life or work. The cost of pain to our nation is estimated between $560 billion and $635 billion annually. At the same time, our nation is facing an opioid crisis that, over the past two decades, has resulted in an unprecedented wave of overdose deaths associated with prescription opioids, heroin, and synthetic opioids.
Patients with acute and chronic pain face a crisis because of challenges in obtaining adequate care, resulting in profound physical, emotional, and societal costs. According to the CDC, 50 million adults in the US have chronic daily pain, with 19.6 million adults experiencing high impact chronic pain that interferes with daily life or work. The cost of pain to our nation is estimated between $560 billion and $635 billion annually. At the same time, our nation is facing an opioid crisis that, over the past two decades, has resulted in an unprecedented wave of overdose deaths associated with prescription opioids, heroin, and synthetic opioids.
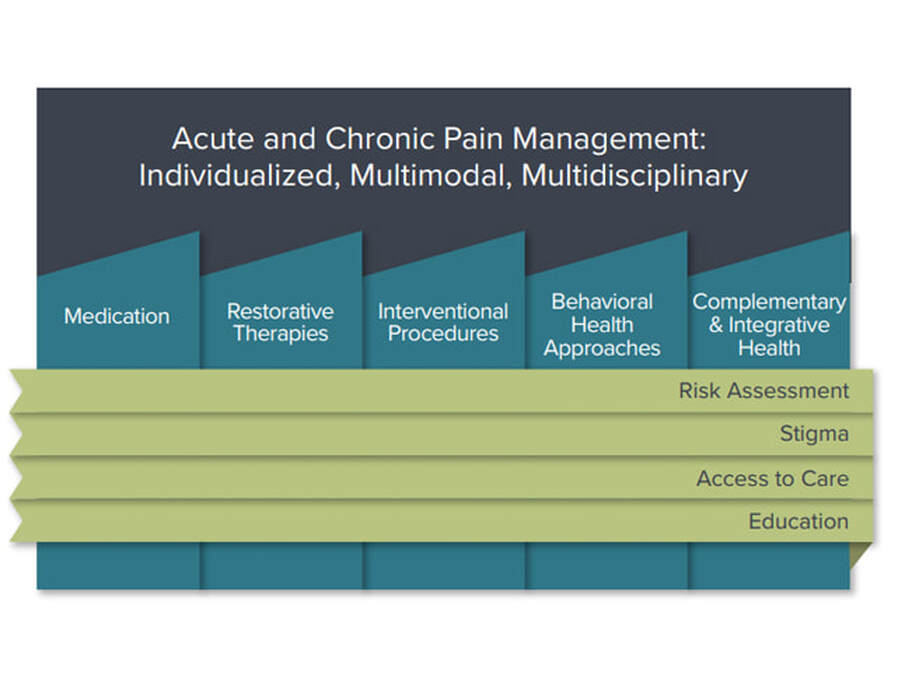
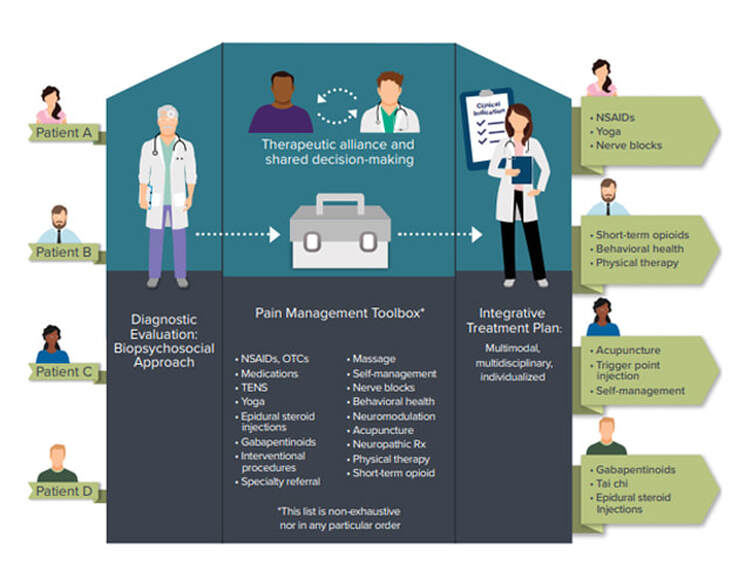
An emphasis on an individualized, patient-centered approach for diagnosis and treatment of pain is essential to establishing a therapeutic alliance between patient and clinician. Acute pain can be caused by a variety of conditions, such as trauma, burn, musculoskeletal injury, and neural injury, as well as pain from surgery or procedures. Health systems and clinicians must consider the pain management needs of every individual.
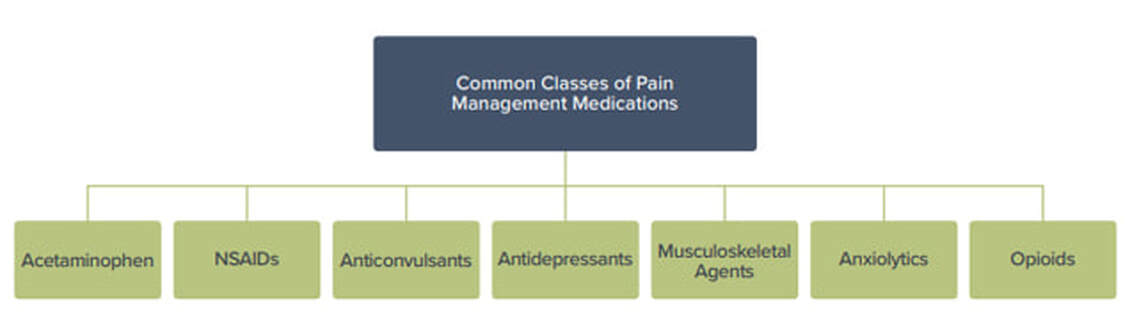
A multidisciplinary approach for chronic pain across various disciplines, using one or more treatment modalities, is encouraged when clinically indicated to improve outcomes. The choice of medication should be based on the pain diagnosis, the mechanisms of pain, and related co-morbidities following a thorough history, physical exam, other relevant diagnostic procedures and a risk-benefit assessment that demonstrates that the benefits of a medication outweigh the risks. The goal is to limit adverse outcomes while ensuring that patients have access to medication-based treatment that can enable a better outcome and function. Various classes of medications, including non-opioids and opioids, should be considered for use.
|
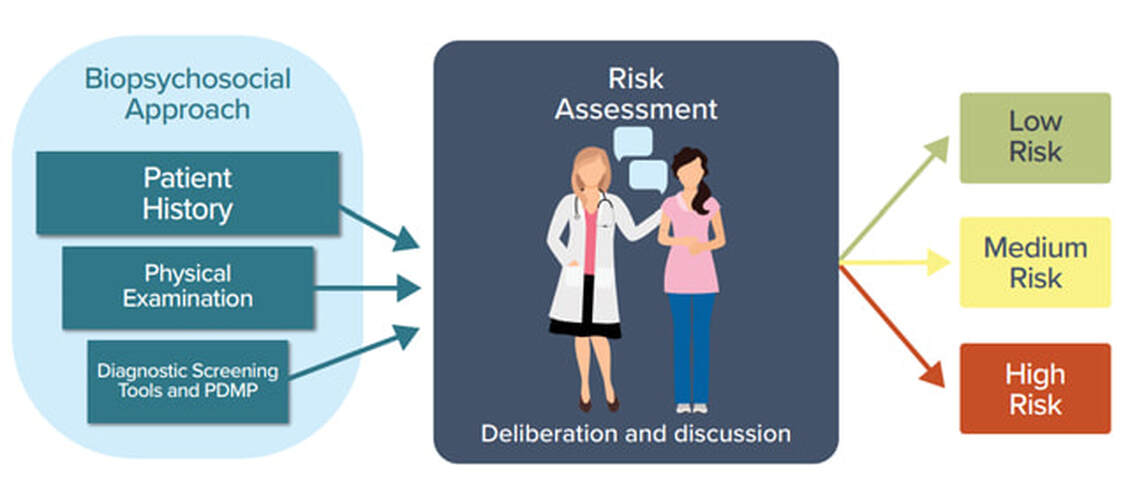
Risk assessment is one of the four cross-cutting policy approaches necessary for best practices in providing individualized, patient-centered care. A thorough patient assessment and evaluation for treatment that includes a risk-benefit analysis are important considerations when developing patient-centered treatment. Risk assessment involves identifying risk factors from patient history; family history; current biopsychosocial factors; and screening and diagnostic tools, including prescription drug monitoring programs, laboratory data, and other measures. Risk stratification for a particular patient can aid in determining appropriate treatments for the best clinical outcomes for that patient. Safe opioid use includes regular reevaluation of the patient. |
|
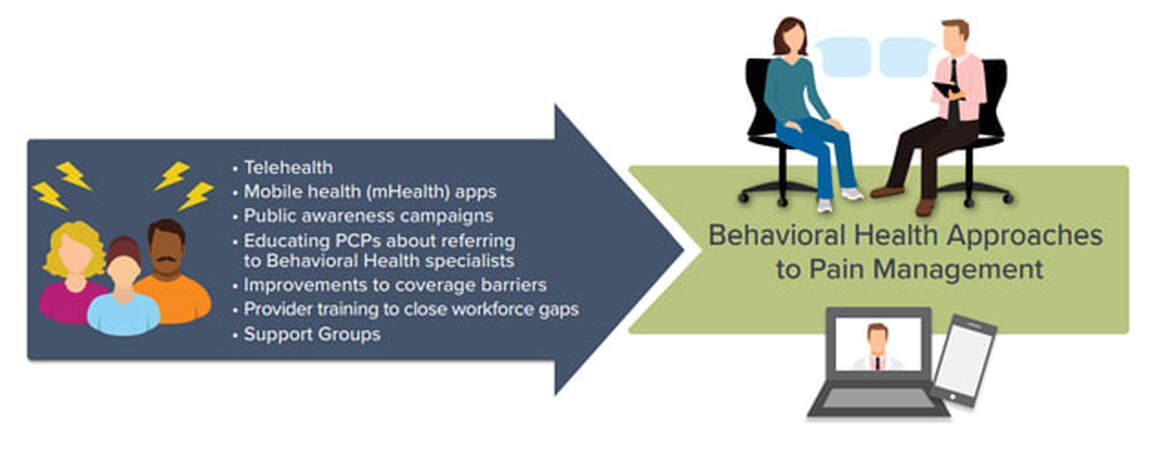
Improved insurance coverage and payment for different pain management modalities is critical to improving access to effective clinical care and should include coverage and payment for care coordination, complex opioid management, and telemedicine. It is also important to note that in many parts of the country, patients have access only to a primary care provider (PCP). Support for education, time, and financial resources for PCPs is essential to managing patients who have painful conditions. A multimodal approach that includes medications, nerve blocks, physical therapy, and other modalities should be considered for acute pain conditions. |
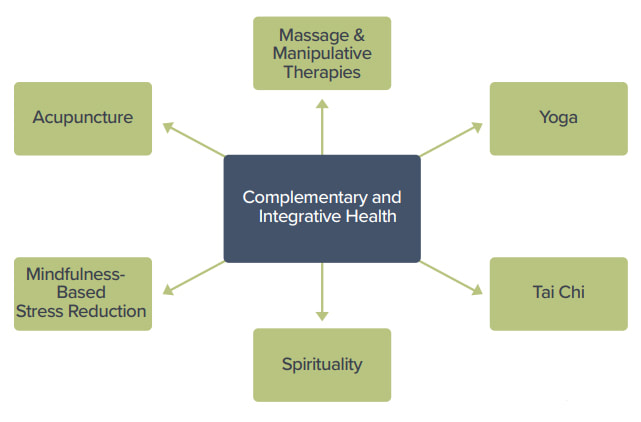
Complementary and Integrative Health, including treatment modalities such as acupuncture, massage, movement therapies (e.g., yoga, tai chi), and spirituality, should be considered when clinically indicated.
|
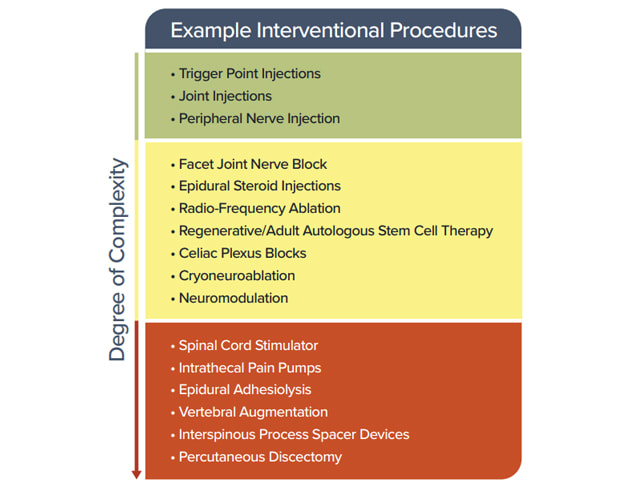
Restorative Therapies, including those implemented by physical therapists and occupational therapists are valuable components of multidisciplinary, multimodal acute and chronic pain care. Interventional Approaches, including image-guided and minimally invasive procedures are available like trigger point injections, radio-frequency ablation, cryo-neuroablation, neuromodulation, and other procedures. |
Behavioral Approaches for psychological, cognitive, emotional, behavioral, and social aspects of pain can have a significant impact on treatment outcomes. Patients with pain and behavioral health comorbidities face challenges that can exacerbate painful conditions as well as function, QOL, and ADLs. Effective multidisciplinary management of the potentially complex aspects of acute and chronic pain should be based on a biopsychosocial model of care.
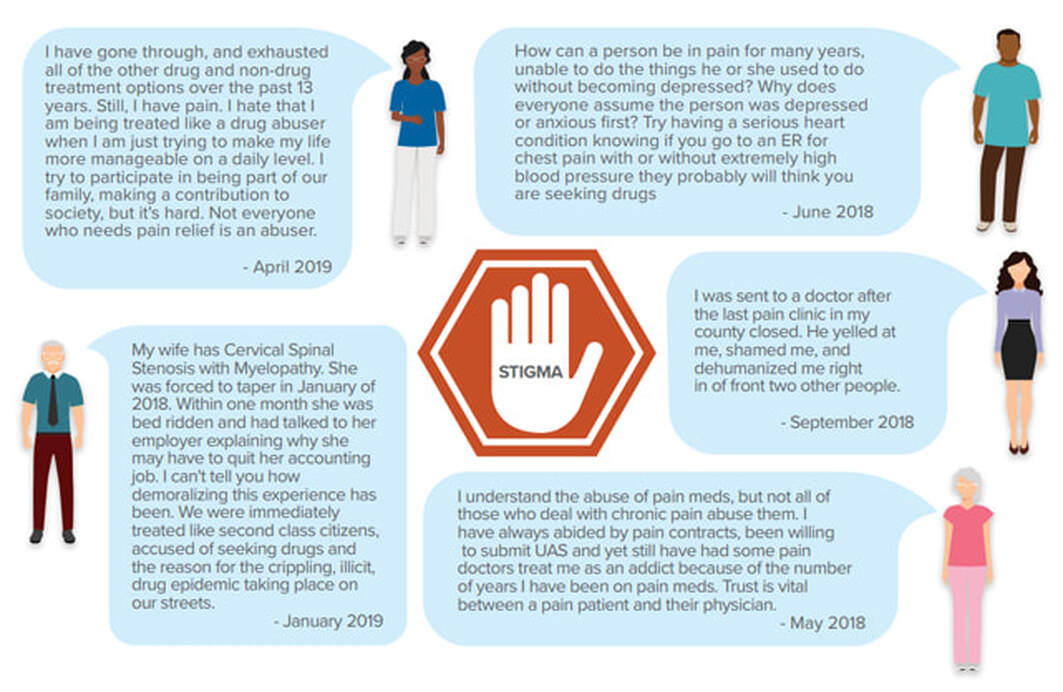
Stigma can be a barrier to treatment of painful conditions. Compassionate, empathetic care centered on a patient-clinician relationship is necessary to counter the suffering of patients with painful conditions and to address the various challenges associated with the stigma of living with pain. Stigma often presents a barrier to care and is often cited as a challenge for patients, families, caregivers, and providers.
Addressing barriers to access to care is essential in optimizing pain care. Recommendations include addressing the gap in
our workforce for all disciplines involved in pain management.
Addressing barriers to access to care is essential in optimizing pain care. Recommendations include addressing the gap in
our workforce for all disciplines involved in pain management.
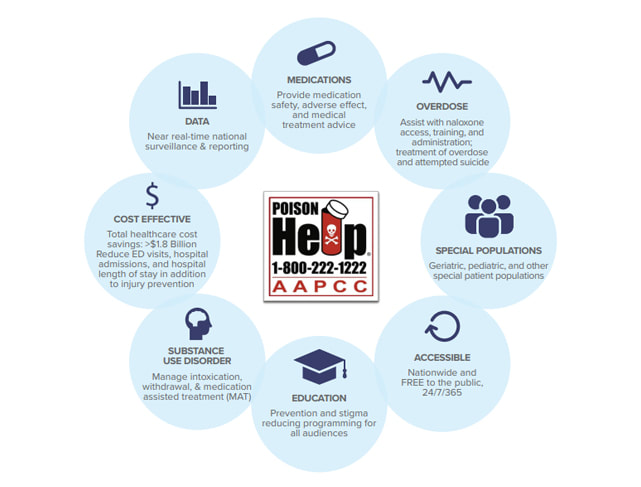
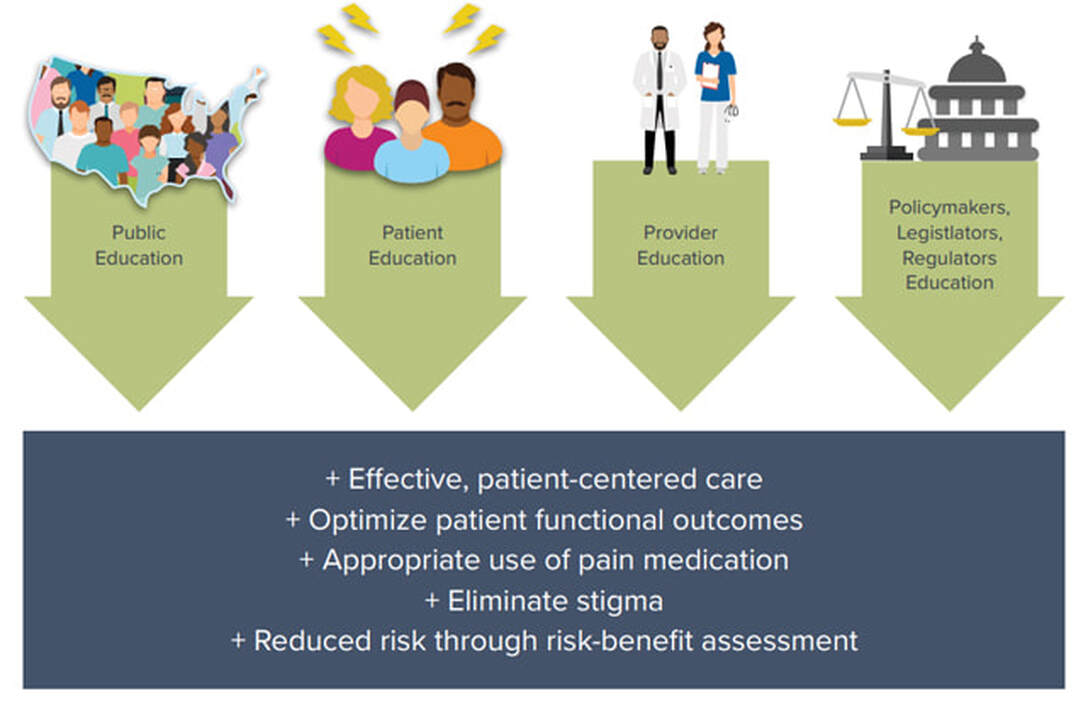
Improving education about pain conditions and their treatment for patients, families, caregivers, clinicians, and policymakers is vital to enhancing pain care. Patient education can be emphasized through various means, including clinician discussion, informational materials, and web resources. More effective education and training about acute and chronic pain should occur at all levels of clinician training, including undergraduate educational curricula, graduate professional training, and continuing professional education.
U.S. Department of Health and Human Services (2019, May). Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations. Retrieved from U. S. Department of Health and Human Services website: https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html