A Story From the Patient Mind Community
A Journey to Hope.
Here you will find education on MDD (Depression). Your educational journey will include animations on symptoms, communication, shared decision-making, and treatment options. It is important to know your management options for healthy dialogue with your healthcare provider. Download the MDD Communication Guide to prepare for your next healthcare visit.
Shared Decision-Making
Click or tap each topic below to understand shared decision-making.
Patient-Centered Healthcare
If you struggle with depression, it is important to be active in your healthcare needs. Your desired outcomes and goals empower you to work along side your healthcare provider during clinical decisions. This is called patient-centered healthcare.
Clinician and Patient Working Together
While the clinician has a job to prescribe the best possible management options, it is your job to adhere to the prescribed management. It is also your job to track and communicate progress or issues you may experience, so both you and your healthcare provider can continue to manage depression as a team.
Treatments and Care Plans Based on Clinical Evidence
Discuss treatment options and care plans with your healthcare provider that are based on clinical evidence. This means research and science have proven that the treatment and care plans work for depression.
Balance Between Risks and Expected Outcomes w/ Patient Preferences and Values
Shared decision-making is a balance between risks and expected outcomes, along with patient preferences and values. This means the healthcare provider and patient discuss and understand risks associated with a management plan and the appropriate expectations. These are aligned with the preference and values of the patient. These can only be established with good communication. Again, the patient and healthcare provider must do their part in communication!
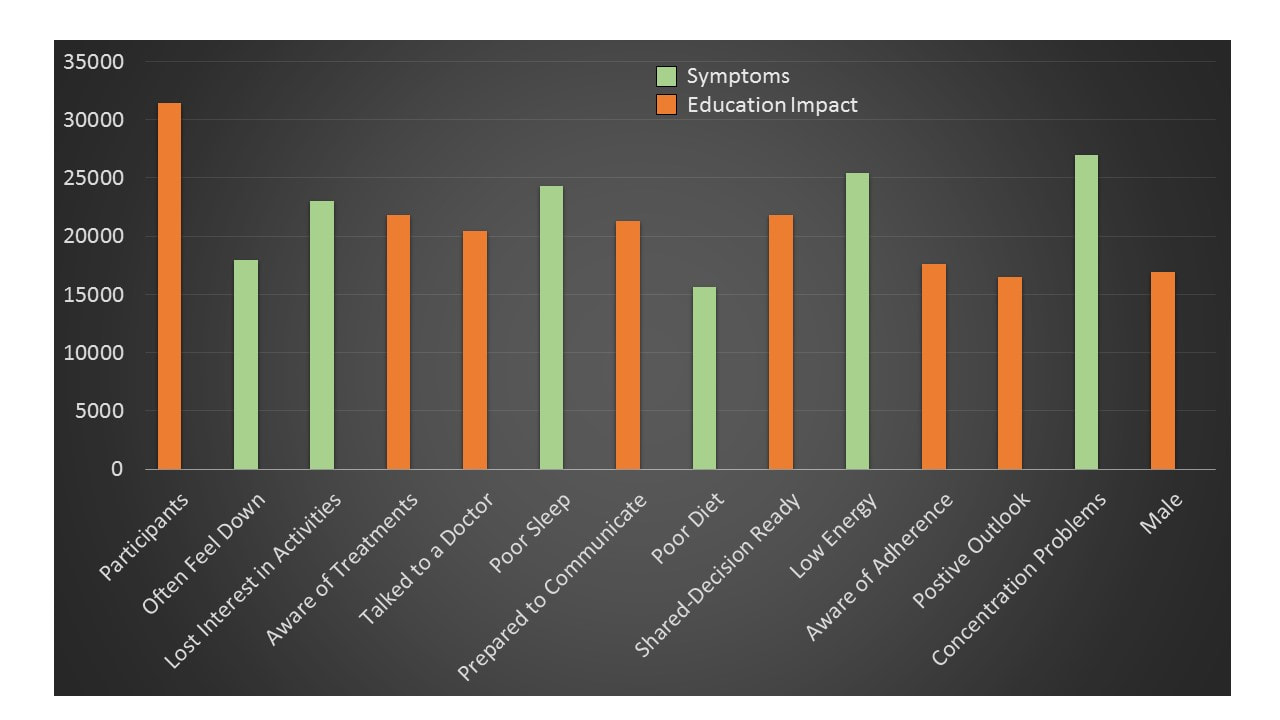
Symptoms and Education Impact
Below are the 2019 non-identifiable results of the Patient Mind Inc. community. Please take the survey to see where you stand with your Depression.
5 Levels of Protection in MDD Management
Understanding MDD is similar to minecraft. Minecraft is an online video game about managing your life's adventure. You are given resources to build your world, and you must explore and defend yourself against threats. We are going to break down and simplify how to do this in real life to manage MDD.
Level 1: Be Mindful
Be mindful of negative thoughts, negative talk, and negative situations, and replace them with positive thoughts and actions.
Level 2: Surround Yourself with Professionals
Surround yourself with professionals... including Primary Care, Psychiatrists, Psychologists, Physical Therapists, Personal Trainers, and/or Dietitians. (Click to find a specialist in your area) That's what they are here for!
Level 3: Treat As Prescribed
Treat MDD with the medications and lifestyles prescribed by the healthcare professionals. See medication options below!
Level 4: Adhere
Adhere and practice relentlessly, until you have a routine that works.
Level 5: Live and Enjoy Life
Laugh, create, volunteer, and give to good causes.
MDD (Antidepressant) MEdications Explained
Click or tap each topic below to understand options your healthcare provider may prescribe. Patient Mind Inc. does not endorse any medication. This is for education purposes only. For Side Effects, Precautions and Interactions, visit the medication links.
|
Vortioxetine (Trintellix)
How it works: Experts believe that depression (MDD) results when certain chemicals in the brain are out of balance. These chemicals, called neurotransmitters, send messages from one brain cell to another by acting at specific receptors. Vortioxetine is thought to work by enhancing the activity of a neurotransmitter called serotonin in the brain by blocking serotonin reuptake. It also has activities on some of the receptors for this brain chemical. The link between this information and the therapeutic benefit is not known. References: vilazdone (Viibryd)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
References:
citalopram (Celexa)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
escitalopram (Lexapro)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
fluoxetine (Prozac, Sarafem, Symbyax)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
fluvoxamine (Luvox, Luvox CR)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
paroxetine (Paxil, Paxil CR, Pexeva)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
sertraline (Zoloft)
A Selective Serotonin Reuptake Inhibitor (SSRI) According to the FDA, you should ask Your Doctor
selEgiline (Emsam)
A MONOAMINE OXIDASE INHIBITOR (MAOI) According to the FDA, you should ask Your Doctor
Isocarboxzaid (Marplan)
A MONOAMINE OXIDASE INHIBITOR (MAOI) According to the FDA, you should ask Your Doctor
Phenelzine (Nardil)
A MONOAMINE OXIDASE INHIBITOR (MAOI) According to the FDA, you should ask Your Doctor
Tranylcypromine (Parnate)
A MONOAMINE OXIDASE INHIBITOR (MAOI) According to the FDA, you should ask Your Doctor
Reference: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/012342s064lbl.pdf Amitriptyline (Amitid, Amitril, Elavil, Endep, Etrafon, Limbitrol, Triavil)
According to the FDA, you should ask Your Doctor
Amoxapine (Asendin)
According to the FDA, you should ask Your Doctor
|
Maprotiline (ludiomil)
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Trazodone (Desyrel)
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Nefazodone
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Mirtazapine
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Bupropion
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Venlafaxine
An Atypical Antidepressant According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Duloxetine (Cymbalta)
A Selective Serotonin and Norepinephrine Reuptake Inhibitor (SNRI) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants Desvenlafaxine (Pristiq)
A Selective Serotonin and Norepinephrine Reuptake Inhibitor (SNRI) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants TRIMIPRAMINE (SURMONTIL)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants PROTRIPTYLINE (VIVACTIL)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants NORTRIPTYLINE (PAMELOR)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants IMIPRAMINE (TOFRANIL)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants DOXEPIN (SINEQUAN)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants DESIPRAMINE (NORPRAMIN)
A Tricyclic Antidepressant (TCA) According to the FDA, you should ask Your Doctor
Reference: https://www.fda.gov/consumers/free-publications-women/depression-medicines-help-you#Atypical_Antidepressants |
Learn From Patient Stories
Click or tap each topic below the name to understand what these other people have experienced
John (A Patient Story)
John's History
John started experiencing symptoms of depression in his late 20's. He became increasingly sad and irritable. John lost interest in activities he usually enjoyed, and shut himself off to many activities.
Talent
John is very talented in photography. His favorite thing to do is photograph nature scenes. But, as his depression came on, his interests were lost and he started to wonder what was wrong.
Medicines
John tracked his depression symptoms so his healthcare provider would realize the impact it is having on his life. He was prescribed a number of antidepressants over the years. He struggled with early antidepressants because of side effects. He became frustrated. In 2019 his healthcare provider told him about new options. It did not work right away, however, now on average he is having 11 less depressed days. With the combination of psychotherapy and antidepressants, he is getting back on track and looks forward to a creative future.
Symptoms
Over six years, John had nine symptoms of depression. These included the following:
- Sadness, Irritability, and Anger
- Lost interest in activities he usually liked
- Weight changes, both gained and loss
- Sleep troubles, both too little and too much
- Restlessness and Low Back Pain
- Lack of energy
- Feelings of worthlessness and guilt
- Trouble concentrating
- Thoughts of self-harm
Exercise
John found that walking daily improves his mood. He enjoys the outdoors and photography, so walking provides him with an enjoyable exercise that he is likely to continue.
Relaxation
John learned to practice biofeedback. This is where he learn to control an automatic body function. For example, when John get's irritable his heart starts to race. By a combination of controlled deep breathing and imagery he can slow his heart rate and relax.
Sleep
John noticed that the lack of sleep, irregular sleep, or too much sleep increases his symptom frequency. Now he practices a regular sleep schedule from 11pm to 7am.
Diet
Certain foods and drinks impact John's mood. For example, excessive pasta and breads make him irritable. Too much alcohol increases his irritability and sleep problems. Unhealthy eating and drinking also makes him feel guilty.
Stages
John feels like he went through different stages of depression and related symptoms. Almost like peaks and valleys. He found it helpful to document these so he can speak with his doctor and be prepared for the high and lows of depression.
Triggers
John now understands that the mind and body are connected. Physical health and mental health go hand-in-hand. Eating healthy, exercise, sleep, and relaxation are important lifestyle techniques. These "protective factors" are likely to achieve total health.
Tracking
John keeps track of his symptoms and protective factors on a smartphone app. This is useful and convenient for dialogue with his doctor at regular clinical visits.
Side Effects
All medications carry precautions, risks, side effects, and interactions. Always consult your healthcare provider for all your healthcare decisions.
Psychotherapy
There are several types of therapy proven to treat symptoms of depression. Many use a combination of techniques:
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
Emma (A Patient Story)
Emma's History
Emma started experiencing symptoms of depression in her late teens. She became increasingly sad and irritable. Emma lost interest in activities she usually enjoyed, and shut herself off from friends.
Talent
Emma is very talented in soccer. Her favorite thing to do is play soccer at a local soccer club. But, as her depression came on, her interests were lost and she started to wonder what was wrong.
Medicines
Emma tracked her depression symptoms so her healthcare provider would realize the impact it is having on her life. She was prescribed a number of antidepressants over the years. She struggled with side effects. In 2019 her healthcare provider told her about other options. She is having 8 less depressed days. With the combination of psychotherapy, lifestyle, and antidepressants, she is getting back on track.
Symptoms
Over six years, Emma had 8 symptoms of depression. These included the following:
- Sadness, Irritability, and Anger
- Lost interest in activities he usually liked
- Weight changes, both gained and loss
- Sleep troubles, both too little and too much
- A feeling of restlessness
- Lack of energy
- Feelings of worthlessness and guilt
- Trouble concentrating
- Thoughts of self-harm
Exercise
Emma found that exercising daily improves her mood. She enjoys practicing soccer, so practice provides her with an enjoyable exercise that she is likely to continue.
Relaxation
Emma learned to practice deep breathing. This is where she calms her nervous system by breathing in for 3 seconds, hold for 2 seconds, and exhales for 3 seconds. She frees her mind of negative thoughts and relaxes her muscles. This can help with depression symptoms.
Sleep
Emma noticed that the lack of sleep, irregular sleep, or too much sleep increases her symptoms. Now she practices a regular sleep schedule from 10pm to 7am.
Diet
Certain foods and drinks impact Emma's mood. For example, excessive sweets make her feel guilty. Too much alcohol increases her sadness and sleep problems.
Stages
Emma feels like depression is like walking though peaks and valleys. She found it helpful to document these so she can speak with her doctor and be prepared for the high and lows of depression.
Triggers
Emma understands her physical health and mental health go hand-in-hand. Eating healthy, exercise, sleep, and relaxation are important lifestyle techniques to achieve total health.
Tracking
Emma tracks her symptoms on a smartphone app. This is useful and convenient for dialogue with her doctor at regular clinical visits.
Side Effects
All medications carry precautions, risks, side effects, and interactions. Always consult your healthcare provider for all your healthcare decisions.
Psychotherapy
There are several types of therapy proven to treat symptoms of depression. Many use a combination of techniques:
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
Morgan (A Patient Story)
Morgan's History
Morgan has experienced symptoms of depression for 40+ years. He went through cycles where he lost interest in activities, and shut himself off from friends. The more he shut himself off, the more symptoms he experienced. He found being proactive and enjoying life is the best remedy. However, it is a challenge to stay active and positive.
Talent
Morgan is a talented fisherman. His favorite things to do are fish tournaments in a local bass club and take his granddaughter fishing. But, as his depression comes around, his interests are lost and he starts to stay home and avoid the things he loves... including family.
Medicines
Morgan tracked his depression symptoms for years. He was prescribed a number of antidepressants, but struggled with adherence. In 2019 his healthcare provider taught him the importance of taking the medication as prescribed. With the combination of relaxation, exercise, healthy diet, and antidepressants, he is experiencing 6 less depressed days per month.
Symptoms
Over 40+ years, Morgan had 9 symptoms of depression. These included the following:
- Irritability and Anger
- Lost interest in activities he usually liked
- Weight changes, both gained and loss
- Sleep troubles, both too little and too much
- Aches and Pain
- Lack of energy
- Feelings of worthlessness and guilt
- Trouble concentrating
- Thoughts of self-harm
Exercise
Morgan found that exercising daily improves his mood. He enjoys fishing, so walking around the lake and scouting new spots are an enjoyable exercise that he is likely to continue.
Relaxation
Morgan learned Progressive Muscle Relaxation. This is where he calms her nervous system by breathing and letting tension go... muscle by muscle. He frees his mind of negative thoughts and it seems to help with depression symptoms and motivation.
Sleep
Morgan noticed that the lack of sleep, irregular sleep, or too much sleep increases his symptoms. Now he practices a regular sleep schedule from 9pm to 5am.
Diet
Certain foods and drinks impact Morgan's mood. For example, excessive fast food makes him tired and irritable. Alcohol increases his sadness and causes sleep problems. Too much caffeine interrupts his sleep also.
Stages
Morgan knows his depression has peaks and valleys. He found it helpful to document these so he can continue to speak with his doctor and be prepared for the high and lows of depression.
Triggers
Morgan understands his physical health and mental health go hand-in-hand. Eating healthy, exercise, sleep, and relaxation are important lifestyle techniques to achieve total health.
Tracking
Morgan tracks his symptoms in a notebook. This is useful and convenient for dialogue with his doctor at regular clinical visits.
Side Effects
All medications carry precautions, risks, side effects, and interactions. Always consult your healthcare provider for all your healthcare decisions.
Psychotherapy
There are several types of therapy proven to treat symptoms of depression. Many use a combination of techniques:
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
Cognitive-behavioral therapy (CBT) identifies and reshapes the thought and behavior patterns that contribute to your depression.
Interpersonal psychotherapy you focuses on your relationships, how you interact with other people in your life, and the different roles you play. Often you learn new ways to interact that can help improve those relationships.
Family and couples therapy is where you attend therapy sessions along with your partner or family members so that you can work together on the issues that are contributing to your depression.
Problem-solving therapy takes a very practical and systematic approach to the problems in your life and find effective ways to solve them.
Psychodynamic therapy explores childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping your current behavior.
If there’s a particular form of psychotherapy that appeals to you, ask a therapist to guide you in doing so.
Clinician guided self-help involves the use of workbooks, audio, or video. People who choose this approach check in periodically with their health care provider but the interactions are much more brief and infrequent compared with formal therapy.
Guided self-help can be a good choice for people who have mild depression and have no thoughts of death or suicide. People who fall into this category can even try self-help approaches on their own, without checking in with a health care provider, unless their symptoms start to get worse.
Reference: Simon G. Retrieved from https://www.uptodate.com/contents/depression-treatment-options-for-adults-beyond-the-basics
What is Depression?
Click or tap the play button to watch an interesting animation on depression.
What is depression? By Helen M. Farrell. Produced by TEDED
Overcoming Depression
Click or tap the play button to watch a inspirational animation on overcoming depression.
Overcomer Animated Short By Hannah Grace.
Depression IQ
Please take the Depression IQ again so we can measure education impact!
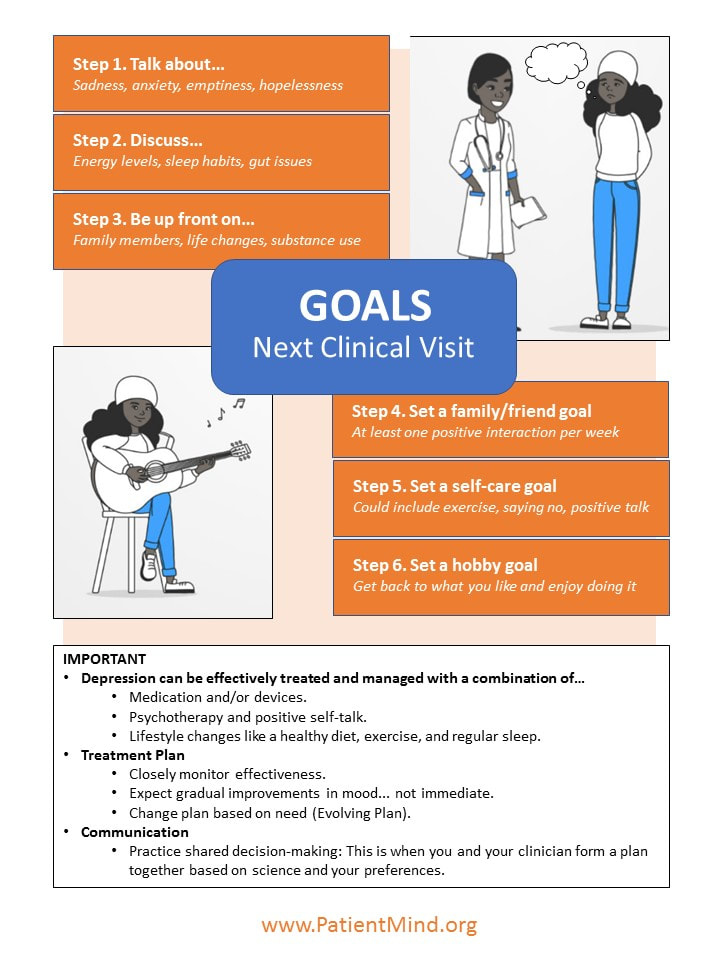
Communication Guide
Download Your Depression Communication Guide for Your Next Clinical Visit!
References
Click Here to expand the references
- Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry 2011; 68:90.
- Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2197.
- Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA 2013; 310:591.
- Solomon DA, Keller MB, Leon AC, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry 2000; 157:229.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), American Psychiatric Association, Arlington 2013.
- HAMILTON M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56.
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382.
- American Psychiatric Association: Practice Guideline for the Treatment of Patients with Major Depressive Disorder, Third Edition, 2010. http://psychiatryonline.org/guidelines.aspx (Accessed on April 17, 2012).
- Cleare A, Pariante CM, Young AH, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol 2015; 29:459.
- Bauer M, Pfennig A, Severus E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry 2013; 14:334.
- Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006; 163:1905.
- Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry 2009; 70:1219.
- Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety 2009; 26:279.
- Kupfer DJ, Frank E, Phillips ML. Major depressive disorder: new clinical, neurobiological, and treatment perspectives. Lancet 2012; 379:1045.
- Cuijpers P, Reynolds CF 3rd, Donker T, et al. Personalized treatment of adult depression: medication, psychotherapy, or both? A systematic review. Depress Anxiety 2012; 29:855.
- Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry 2010; 67:1265.
- Givens JL, Houston TK, Van Voorhees BW, et al. Ethnicity and preferences for depression treatment. Gen Hosp Psychiatry 2007; 29:182.
- National Institute for Health & Clinical Excellence. The Treatment and Management of Depression in Adults (updated edition). National Clinical Practice Guideline 90, 2010. http://www.nice.org.uk/ (Accessed on December 09, 2012).
- Cuijpers P, Sijbrandij M, Koole SL, et al. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry 2014; 13:56.
- Cuijpers P, van Straten A, Hollon SD, Andersson G. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: a meta-analysis. Acta Psychiatr Scand 2010; 121:415.
- Thase ME, Greenhouse JB, Frank E, et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry 1997; 54:1009.
- Levkovitz Y, Tedeschini E, Papakostas GI. Efficacy of antidepressants for dysthymia: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry 2011; 72:509.
- Cipriani A, Barbui C, Butler R, et al. Depression in adults: drug and physical treatments. BMJ Clin Evid 2011; 2011.
- Papakostas GI, Fava M. Does the probability of receiving placebo influence clinical trial outcome? A meta-regression of double-blind, randomized clinical trials in MDD. Eur Neuropsychopharmacol 2009; 19:34.
- Singh SP, Singh V, Kar N. Efficacy of agomelatine in major depressive disorder: meta-analysis and appraisal. Int J Neuropsychopharmacol 2012; 15:417.
- Leucht C, Huhn M, Leucht S. Amitriptyline versus placebo for major depressive disorder. Cochrane Database Syst Rev 2012; 12:CD009138.
- Cipriani A, Purgato M, Furukawa TA, et al. Citalopram versus other anti-depressive agents for depression. Cochrane Database Syst Rev 2012; :CD006534.
- Girardi P, Pompili M, Innamorati M, et al. Duloxetine in acute major depression: review of comparisons to placebo and standard antidepressants using dissimilar methods. Hum Psychopharmacol 2009; 24:177.
- Cipriani A, Santilli C, Furukawa TA, et al. Escitalopram versus other antidepressive agents for depression. Cochrane Database Syst Rev 2009; :CD006532.
- Undurraga J, Tondo L, Schalkwijk S, et al. Re-analysis of the earliest controlled trials of imipramine. J Affect Disord 2013; 147:451.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; :CD006528.
- Barbui C, Furukawa TA, Cipriani A. Effectiveness of paroxetine in the treatment of acute major depression in adults: a systematic re-examination of published and unpublished data from randomized trials. CMAJ 2008; 178:296.
- Cipriani A, La Ferla T, Furukawa TA, et al. Sertraline versus other antidepressive agents for depression. Cochrane Database Syst Rev 2010; :CD006117.
- Thase ME, Trivedi MH, Rush AJ. MAOIs in the contemporary treatment of depression. Neuropsychopharmacology 1995; 12:185.
- Arroll B, Elley CR, Fishman T, et al. Antidepressants versus placebo for depression in primary care. Cochrane Database Syst Rev 2009; :CD007954.
- Storosum JG, Elferink AJ, van Zwieten BJ, et al. Short-term efficacy of tricyclic antidepressants revisited: a meta-analytic study. Eur Neuropsychopharmacol 2001; 11:173.
- Leucht S, Hierl S, Kissling W, et al. Putting the efficacy of psychiatric and general medicine medication into perspective: review of meta-analyses. Br J Psychiatry 2012; 200:97.
- Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry 2012; 69:572.
- Thase ME. The small specific effects of antidepressants in clinical trials: what do they mean to psychiatrists? Curr Psychiatry Rep 2011; 13:476.
- Posternak MA, Zimmerman M. Therapeutic effect of follow-up assessments on antidepressant and placebo response rates in antidepressant efficacy trials: meta-analysis. Br J Psychiatry 2007; 190:287.
- Leuchter AF, McCracken JT, Hunter AM, et al. Monoamine oxidase a and catechol-o-methyltransferase functional polymorphisms and the placebo response in major depressive disorder. J Clin Psychopharmacol 2009; 29:372.
- Melander H, Salmonson T, Abadie E, van Zwieten-Boot B. A regulatory Apologia--a review of placebo-controlled studies in regulatory submissions of new-generation antidepressants. Eur Neuropsychopharmacol 2008; 18:623.
- Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med 2008; 358:252.
- Driessen E, Cuijpers P, Hollon SD, Dekker JJ. Does pretreatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J Consult Clin Psychol 2010; 78:668.
- Cuijpers P, Huibers M, Ebert DD, et al. How much psychotherapy is needed to treat depression? A metaregression analysis. J Affect Disord 2013; 149:1.
- Cuijpers P, Karyotaki E, Weitz E, et al. The effects of psychotherapies for major depression in adults on remission, recovery and improvement: a meta-analysis. J Affect Disord 2014; 159:118.
- Cuijpers P, van Straten A, Bohlmeijer E, et al. The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size. Psychol Med 2010; 40:211.
- Cuijpers P, Smit F, Bohlmeijer E, et al. Efficacy of cognitive-behavioural therapy and other psychological treatments for adult depression: meta-analytic study of publication bias. Br J Psychiatry 2010; 196:173.
- Driessen E, Hollon SD, Bockting CL, et al. Does Publication Bias Inflate the Apparent Efficacy of Psychological Treatment for Major Depressive Disorder? A Systematic Review and Meta-Analysis of US National Institutes of Health-Funded Trials. PLoS One 2015; 10:e0137864.
- Spielmans GI, Berman MI, Usitalo AN. Psychotherapy versus second-generation antidepressants in the treatment of depression: a meta-analysis. J Nerv Ment Dis 2011; 199:142.
- Cuijpers P, Sijbrandij M, Koole SL, et al. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry 2013; 12:137.
- Amick HR, Gartlehner G, Gaynes BN, et al. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ 2015; 351:h6019.
- Cuijpers P, van Straten A, van Oppen P, Andersson G. Are psychological and pharmacologic interventions equally effective in the treatment of adult depressive disorders? A meta-analysis of comparative studies. J Clin Psychiatry 2008; 69:1675.
- Parikh SV, Segal ZV, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. J Affect Disord 2009; 117 Suppl 1:S15.
- Imel ZE, Malterer MB, McKay KM, Wampold BE. A meta-analysis of psychotherapy and medication in unipolar depression and dysthymia. J Affect Disord 2008; 110:197.
- Simon GE, Perlis RH. Personalized medicine for depression: can we match patients with treatments? Am J Psychiatry 2010; 167:1445.
- Narasimhan S, Lohoff FW. Pharmacogenetics of antidepressant drugs: current clinical practice and future directions. Pharmacogenomics 2012; 13:441.
- Garriock HA, Kraft JB, Shyn SI, et al. A genomewide association study of citalopram response in major depressive disorder. Biol Psychiatry 2010; 67:133.
- McMahon FJ. Pioneering first steps and cautious conclusions. Biol Psychiatry 2010; 67:99.
- Leuchter AF, Cook IA, Gilmer WS, et al. Effectiveness of a quantitative electroencephalographic biomarker for predicting differential response or remission with escitalopram and bupropion in major depressive disorder. Psychiatry Res 2009; 169:132.
- Wong ML, Dong C, Flores DL, et al. Clinical outcomes and genome-wide association for a brain methylation site in an antidepressant pharmacogenetics study in Mexican Americans. Am J Psychiatry 2014; 171:1297.
- Crowther A, Smoski MJ, Minkel J, et al. Resting-state connectivity predictors of response to psychotherapy in major depressive disorder. Neuropsychopharmacology 2015; 40:1659.
- Schatzberg AF, DeBattista C, Lazzeroni LC, et al. ABCB1 Genetic Effects on Antidepressant Outcomes: A Report From the iSPOT-D Trial. Am J Psychiatry 2015; 172:751.
- GENDEP Investigators, MARS Investigators, STAR*D Investigators. Common genetic variation and antidepressant efficacy in major depressive disorder: a meta-analysis of three genome-wide pharmacogenetic studies. Am J Psychiatry 2013; 170:207.
- Phillips ML, Chase HW, Sheline YI, et al. Identifying predictors, moderators, and mediators of antidepressant response in major depressive disorder: neuroimaging approaches. Am J Psychiatry 2015; 172:124.
- Bagby RM, Quilty LC, Segal ZV, et al. Personality and differential treatment response in major depression: a randomized controlled trial comparing cognitive-behavioural therapy and pharmacotherapy. Can J Psychiatry 2008; 53:361.
- Fournier JC, DeRubeis RJ, Shelton RC, et al. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. Br J Psychiatry 2008; 192:124.
- Mojtabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. J Clin Psychiatry 2008; 69:1064.
- Spijker J, Nolen WA. An algorithm for the pharmacological treatment of depression. Acta Psychiatr Scand 2010; 121:180.
- Gartlehner G, Hansen RA, Morgan LC, et al. Comparative benefits and harms of second-generation antidepressants for treating major depressive disorder: an updated meta-analysis. Ann Intern Med 2011; 155:772.
- Malhi GS, Hitching R, Berk M, et al. Pharmacological management of unipolar depression. Acta Psychiatr Scand Suppl 2013; :6.
- Lester H, Gilbody S. Choosing a second generation antidepressant for treatment of major depressive disorder. BMJ 2012; 344:e1014.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-Generation Antidepressants in the Pharmacologic Treatment of Adult Depression: An Update of the 2007 Comparative Effectiveness Review. AHRQ Publication No. 12-EHC012-EF. PMID 22299185. http://effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/ (Accessed on June 01, 2018).
- Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 2009; 373:746.
- Qaseem A, Snow V, Denberg TD, et al. Using second-generation antidepressants to treat depressive disorders: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2008; 149:725.
- Gartlehner G, Thaler K, Hill S, Hansen RA. How should primary care doctors select which antidepressants to administer? Curr Psychiatry Rep 2012; 14:360.
- Thaler KJ, Morgan LC, Van Noord M, et al. Comparative effectiveness of second-generation antidepressants for accompanying anxiety, insomnia, and pain in depressed patients: a systematic review. Depress Anxiety 2012; 29:495.
- Papakostas GI, Stahl SM, Krishen A, et al. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry 2008; 69:1287.
- Uher R, Tansey KE, Dew T, et al. An inflammatory biomarker as a differential predictor of outcome of depression treatment with escitalopram and nortriptyline. Am J Psychiatry 2014; 171:1278.
- Andersohn F, Schade R, Suissa S, Garbe E. Long-term use of antidepressants for depressive disorders and the risk of diabetes mellitus. Am J Psychiatry 2009; 166:591.
- Atlantis E, Browning C, Sims J, Kendig H. Diabetes incidence associated with depression and antidepressants in the Melbourne Longitudinal Studies on Healthy Ageing (MELSHA). Int J Geriatr Psychiatry 2010; 25:688.
- Wu CS, Wang SC, Cheng YC, Gau SS. Association of cerebrovascular events with antidepressant use: a case-crossover study. Am J Psychiatry 2011; 168:511.
- Voican CS, Corruble E, Naveau S, Perlemuter G. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry 2014; 171:404.
- Wu CH, Farley JF, Gaynes BN. The association between antidepressant dosage titration and medication adherence among patients with depression. Depress Anxiety 2012; 29:506.
- Ruhé HG, Huyser J, Swinkels JA, Schene AH. Dose escalation for insufficient response to standard-dose selective serotonin reuptake inhibitors in major depressive disorder: systematic review. Br J Psychiatry 2006; 189:309.
- Shelton RC, Osuntokun O, Heinloth AN, Corya SA. Therapeutic options for treatment-resistant depression. CNS Drugs 2010; 24:131.
- Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord 2009; 117 Suppl 1:S26.
- Jakubovski E, Varigonda AL, Freemantle N, et al. Systematic Review and Meta-Analysis: Dose-Response Relationship of Selective Serotonin Reuptake Inhibitors in Major Depressive Disorder. Am J Psychiatry 2016; 173:174.
- Drozda K, Müller DJ, Bishop JR. Pharmacogenomic testing for neuropsychiatric drugs: current status of drug labeling, guidelines for using genetic information, and test options. Pharmacotherapy 2014; 34:166.
- D'Empaire I, Guico-Pabia CJ, Preskorn SH. Antidepressant treatment and altered CYP2D6 activity: are pharmacokinetic variations clinically relevant? J Psychiatr Pract 2011; 17:330.
- Uher R, Mors O, Rietschel M, et al. Early and delayed onset of response to antidepressants in individual trajectories of change during treatment of major depression: a secondary analysis of data from the Genome-Based Therapeutic Drugs for Depression (GENDEP) study. J Clin Psychiatry 2011; 72:1478.
- Posternak MA, Zimmerman M. Is there a delay in the antidepressant effect? A meta-analysis. J Clin Psychiatry 2005; 66:148.
- Papakostas GI, Perlis RH, Scalia MJ, et al. A meta-analysis of early sustained response rates between antidepressants and placebo for the treatment of major depressive disorder. J Clin Psychopharmacol 2006; 26:56.
- Taylor MJ, Freemantle N, Geddes JR, Bhagwagar Z. Early onset of selective serotonin reuptake inhibitor antidepressant action: systematic review and meta-analysis. Arch Gen Psychiatry 2006; 63:1217.
- Stassen HH, Angst J, Hell D, et al. Is there a common resilience mechanism underlying antidepressant drug response? Evidence from 2848 patients. J Clin Psychiatry 2007; 68:1195.
- Katz MM, Meyers AL, Prakash A, et al. Early symptom change prediction of remission in depression treatment. Psychopharmacol Bull 2009; 42:94.
- Ciudad A, Álvarez E, Roca M, et al. Early response and remission as predictors of a good outcome of a major depressive episode at 12-month follow-up: a prospective, longitudinal, observational study. J Clin Psychiatry 2012; 73:185.
- Jakubovski E, Bloch MH. Prognostic subgroups for citalopram response in the STAR*D trial. J Clin Psychiatry 2014; 75:738.
- Szegedi A, Jansen WT, van Willigenburg AP, et al. Early improvement in the first 2 weeks as a predictor of treatment outcome in patients with major depressive disorder: a meta-analysis including 6562 patients. J Clin Psychiatry 2009; 70:344.
- Rush AJ. STAR*D: what have we learned? Am J Psychiatry 2007; 164:201.
- Papakostas GI. Managing partial response or nonresponse: switching, augmentation, and combination strategies for major depressive disorder. J Clin Psychiatry 2009; 70 Suppl 6:16.
- Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 2003; 53:649.
- McIntyre RS. When should you move beyond first-line therapy for depression? J Clin Psychiatry 2010; 71 Suppl 1:16.
- Papakostas GI, Thase ME, Fava M, et al. Are antidepressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agents. Biol Psychiatry 2007; 62:1217.
- Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006; 163:28.
- Quitkin FM, Petkova E, McGrath PJ, et al. When should a trial of fluoxetine for major depression be declared failed? Am J Psychiatry 2003; 160:734.
- Posternak MA, Baer L, Nierenberg AA, Fava M. Response rates to fluoxetine in subjects who initially show no improvement. J Clin Psychiatry 2011; 72:949.
- Romera I, Pérez V, Menchón JM, et al. Early switch strategy in patients with major depressive disorder: a double-blind, randomized study. J Clin Psychopharmacol 2012; 32:479.
- Nierenberg AA, McLean NE, Alpert JE, et al. Early nonresponse to fluoxetine as a predictor of poor 8-week outcome. Am J Psychiatry 1995; 152:1500.
- Crowley RA, Kirschner N, Health and Public Policy Committee of the American College of Physicians. The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: executive summary of an American College of Physicians position paper. Ann Intern Med 2015; 163:298.
- Churchill R, Moore TH, Furukawa TA, et al. 'Third wave' cognitive and behavioural therapies versus treatment as usual for depression. Cochrane Database Syst Rev 2013; :CD008705.
- Hunot V, Moore TH, Caldwell DM, et al. 'Third wave' cognitive and behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst Rev 2013; :CD008704.
- Bell AC, D'Zurilla TJ. Problem-solving therapy for depression: a meta-analysis. Clin Psychol Rev 2009; 29:348.
- Malouff JM, Thorsteinsson EB, Schutte NS. The efficacy of problem solving therapy in reducing mental and physical health problems: a meta-analysis. Clin Psychol Rev 2007; 27:46.
- Cuijpers P, van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol 2008; 76:909.
- Shinohara K, Honyashiki M, Imai H, et al. Behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst Rev 2013; :CD008696.
- Khan A, Faucett J, Lichtenberg P, et al. A systematic review of comparative efficacy of treatments and controls for depression. PLoS One 2012; 7:e41778.
- Hollon SD, Ponniah K. A review of empirically supported psychological therapies for mood disorders in adults. Depress Anxiety 2010; 27:891.
- Lampe L, Coulston CM, Berk L. Psychological management of unipolar depression. Acta Psychiatr Scand Suppl 2013; :24.
- Lemmens LH, Arntz A, Peeters F, et al. Clinical effectiveness of cognitive therapy v. interpersonal psychotherapy for depression: results of a randomized controlled trial. Psychol Med 2015; 45:2095.
- Barth J, Munder T, Gerger H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLoS Med 2013; 10:e1001454.
- Barber JP, Stratt R, Halperin G, Connolly MB. Supportive techniques: are they found in different therapies? J Psychother Pract Res 2001; 10:165.
- Driessen E, Cuijpers P, de Maat SC, et al. The efficacy of short-term psychodynamic psychotherapy for depression: a meta-analysis. Clin Psychol Rev 2010; 30:25.
- Dimidjian S, Davis KJ. Newer variations of cognitive-behavioral therapy: behavioral activation and mindfulness-based cognitive therapy. Curr Psychiatry Rep 2009; 11:453.
- Gellatly J, Bower P, Hennessy S, et al. What makes self-help interventions effective in the management of depressive symptoms? Meta-analysis and meta-regression. Psychol Med 2007; 37:1217.
- Josephine K, Josefine L, Philipp D, et al. Internet- and mobile-based depression interventions for people with diagnosed depression: A systematic review and meta-analysis. J Affect Disord 2017; 223:28.
- Bower P, Kontopantelis E, Sutton A, et al. Influence of initial severity of depression on effectiveness of low intensity interventions: meta-analysis of individual patient data. BMJ 2013; 346:f540.
- Jorm AF, Morgan AJ, Hetrick SE. Relaxation for depression. Cochrane Database Syst Rev 2008; :CD007142.
- Trangle M, Dieperink B, Gabert T, et al. Institute for Clinical Systems Improvement. Major Depression in Adults in Primary Care. Updated May 2012. http://www.icsi.org/depression_5/depression__major__in_adults_in_primary_care_3.html (Accessed on December 12, 2012).
- Rethorst CD, Trivedi MH. Evidence-based recommendations for the prescription of exercise for major depressive disorder. J Psychiatr Pract 2013; 19:204.
- Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev 2013; :CD004366.
- Krogh J, Nordentoft M, Sterne JA, Lawlor DA. The effect of exercise in clinically depressed adults: systematic review and meta-analysis of randomized controlled trials. J Clin Psychiatry 2011; 72:529.
- Krogh J, Videbech P, Thomsen C, et al. DEMO-II trial. Aerobic exercise versus stretching exercise in patients with major depression-a randomised clinical trial. PLoS One 2012; 7:e48316.
- Chalder M, Wiles NJ, Campbell J, et al. Facilitated physical activity as a treatment for depressed adults: randomised controlled trial. BMJ 2012; 344:e2758.
- Schramm E, van Calker D, Dykierek P, et al. An intensive treatment program of interpersonal psychotherapy plus pharmacotherapy for depressed inpatients: acute and long-term results. Am J Psychiatry 2007; 164:768.
- FDA Executive Summary: Prepared for the January 27-28, 2011 meeting of the Neurological Devices Panel. Meeting to Discuss the Classification of Electroconvulsive Therapy Devices (ECT). http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/NeurologicalDevicesPanel/UCM240933.pdf (Accessed on May 25, 2011).
- UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 2003; 361:799.
- Kho KH, van Vreeswijk MF, Simpson S, Zwinderman AH. A meta-analysis of electroconvulsive therapy efficacy in depression. J ECT 2003; 19:139.
- Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT 2004; 20:13.
- Sackeim HA, Haskett RF, Mulsant BH, et al. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trial. JAMA 2001; 285:1299.
- Kellner CH, Knapp RG, Petrides G, et al. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: a multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry 2006; 63:1337.
- Kennedy SH, Milev R, Giacobbe P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) Clinical guidelines for the management of major depressive disorder in adults. IV. Neurostimulation therapies. J Affect Disord 2009; 117 Suppl 1:S44.
- Schuch FB, Vasconcelos-Moreno MP, Borowsky C, et al. Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J Psychiatr Res 2015; 61:25.
- Kerling A, Tegtbur U, Gützlaff E, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord 2015; 177:1.
- Güzel Özdemir P, Boysan M, Smolensky MH, et al. Comparison of venlafaxine alone versus venlafaxine plus bright light therapy combination for severe major depressive disorder. J Clin Psychiatry 2015; 76:e645.
- Nemeroff CB. The burden of severe depression: a review of diagnostic challenges and treatment alternatives. J Psychiatr Res 2007; 41:189.
- Bradley AJ, Lenox-Smith AJ. Does adding noradrenaline reuptake inhibition to selective serotonin reuptake inhibition improve efficacy in patients with depression? A systematic review of meta-analyses and large randomised pragmatic trials. J Psychopharmacol 2013; 27:740.
- Schmitt AB, Bauer M, Volz HP, et al. Differential effects of venlafaxine in the treatment of major depressive disorder according to baseline severity. Eur Arch Psychiatry Clin Neurosci 2009; 259:329.
- Machado M, Iskedjian M, Ruiz I, Einarson TR. Remission, dropouts, and adverse drug reaction rates in major depressive disorder: a meta-analysis of head-to-head trials. Curr Med Res Opin 2006; 22:1825.
- van Moffaert M, de Wilde J, Vereecken A, et al. Mirtazapine is more effective than trazodone: a double-blind controlled study in hospitalized patients with major depression. Int Clin Psychopharmacol 1995; 10:3.
- Guelfi JD, Ansseau M, Timmerman L, et al. Mirtazapine versus venlafaxine in hospitalized severely depressed patients with melancholic features. J Clin Psychopharmacol 2001; 21:425.
- Guaiana G, Barbui C, Hotopf M. Amitriptyline for depression. Cochrane Database Syst Rev 2007; :CD004186.
- Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. Depress Anxiety 1998; 7 Suppl 1:11.
- Cuijpers P, van Straten A, Schuurmans J, et al. Psychotherapy for chronic major depression and dysthymia: a meta-analysis. Clin Psychol Rev 2010; 30:51.
- von Wolff A, Hölzel LP, Westphal A, et al. Selective serotonin reuptake inhibitors and tricyclic antidepressants in the acute treatment of chronic depression and dysthymia: a systematic review and meta-analysis. J Affect Disord 2013; 144:7.
- Kriston L, von Wolff A, Westphal A, et al. Efficacy and acceptability of acute treatments for persistent depressive disorder: a network meta-analysis. Depress Anxiety 2014; 31:621.
- Nemeroff CB, Heim CM, Thase ME, et al. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci U S A 2003; 100:14293.
- Suppes T, Silva R, Cucchiaro J, et al. Lurasidone for the Treatment of Major Depressive Disorder With Mixed Features: A Randomized, Double-Blind, Placebo-Controlled Study. Am J Psychiatry 2016; 173:400.